Key Takeaways
- Healthtech software must be clinically and operationally “doable” – aligned with real clinical workflows, NHS and regulatory requirements, and realistic implementation constraints.
- Tunable, adaptive systems outperform static apps by letting teams configure workflows, dashboards, and AI‑driven journeys to local needs without constant rewrites.
- Renewable platforms treat your app as a long‑term product, using modular architectures and content separation so you can update guidelines, algorithms, and integrations safely over time.
- High‑quality, explainable health data and analytics turn digital tools into real interventions, supporting better decisions, earlier detection, and measurable impact on outcomes.
- Human‑centred, inclusive design that considers clinicians and diverse patient groups remains the strongest predictor of trust, adoption, and long‑term engagement.
Why healthtech software feels hard?
Healthcare apps and platforms sit in one of the most demanding environments for any software development company: high regulatory pressure, complex workflows, and users with very little time or patience. Custom healthcare software needs to balance clinical safety, data protection, and user experience from day one, not as an afterthought. This is why many organisations partner with healthtech‑focused development teams rather than trying to repurpose generic IT vendors.
If you are operating in the UK, building digital products for the NHS or private providers means navigating frameworks such as UK MDR, MHRA guidance, and GDPR – all while proving that your solution is usable in real clinical settings. Our previous article on compliance in healthtech software development walks through why “compliance as a product feature” is now the norm rather than the exception.

Make your product truly “doable” (clinically, technically, organisationally, financially)
A good concept is not enough if your app cannot be safely deployed into everyday healthcare workflows. For UK‑focused solutions, that means aligning early with NHS Digital standards, clinical safety requirements, and data protection expectations under GDPR. Treat your roadmap, architecture, and UX decisions as part of a single clinical safety story rather than disconnected tracks.
On the operational side, realistic integration is key. Custom healthtech platforms that work well usually plug into existing EHR systems, respect local procurement rules, and support phased rollouts across trusts or regions. This is where a healthtech software development company can help you scope APIs, interoperability strategies, and migration plans before a single line of code is written.
What this means for different stakeholders
- Clinicians: Workflows, alerts, and documentation must fit into real clinic or ward routines, not add extra clicks or duplicate data entry.
- IT and engineering teams: Integrations with EHR/PAS, identity systems, and networks need to be realistic given existing infrastructure and security constraints.
- Health leaders and finance teams: There should be a clear business case, including implementation costs, licence or hosting fees, and measurable impact on outcomes or efficiency.
- Patients and carers: Onboarding and everyday use have to feel simple: clear instructions, low cognitive load, and paths for support if something goes wrong.
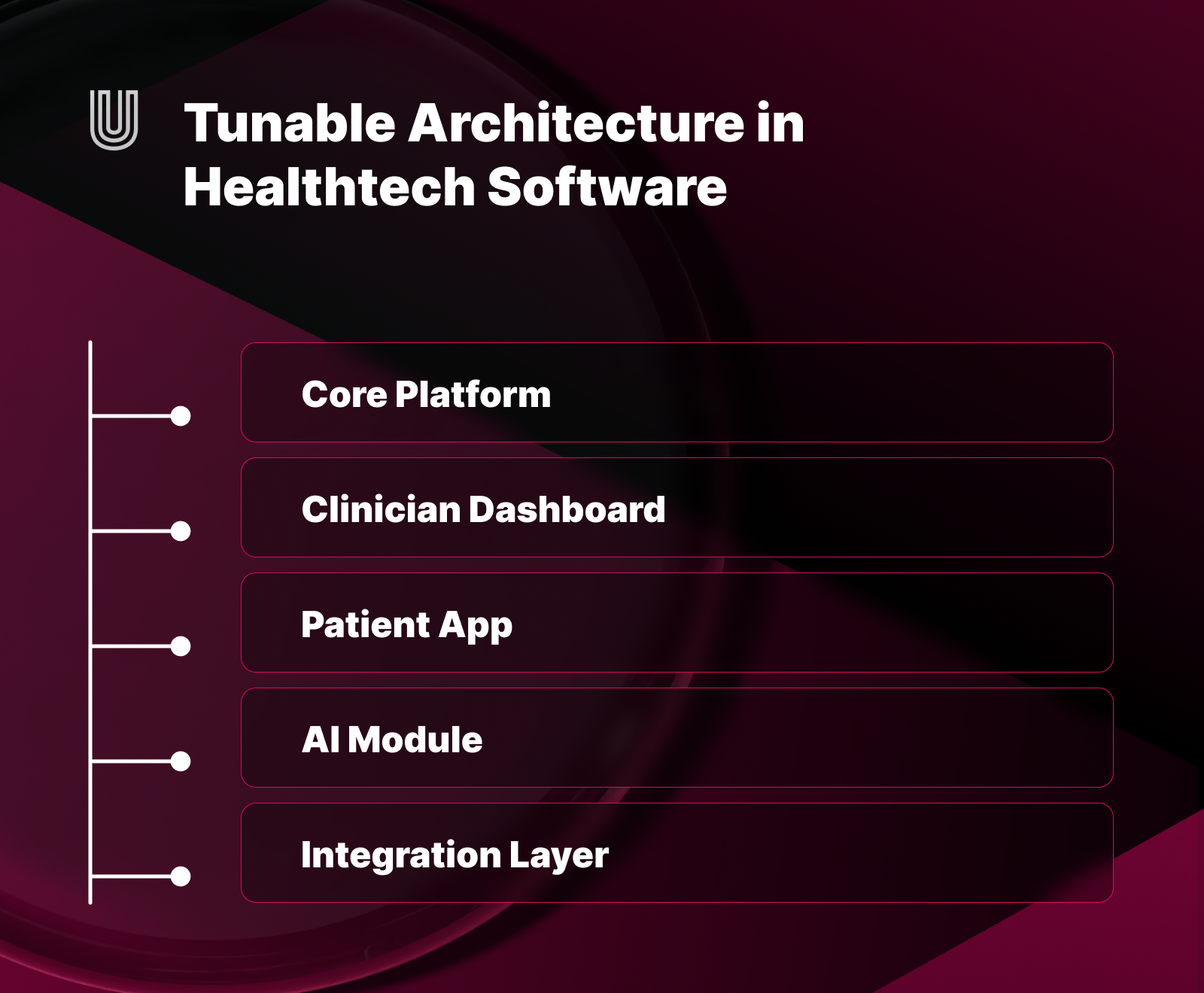
Build tunable and adaptive systems, not static apps
Health apps that cannot flex quickly end up abandoned by both clinicians and patients. Tunable systems let care teams configure workflows, alerts, and dashboards to match local priorities while keeping a consistent core product. For example, one NHS trust may prioritise waiting list management while another needs bed occupancy insights – the same platform can serve both with configurable modules and role‑based views.
AI and data‑driven personalisation push this further. Instead of hard‑coded “one size fits all” journeys, modern digital health products can adapt to patient risk profiles, engagement patterns, and clinical rules over time. This is where working with engineers experienced in AI‑ready healthcare architectures matters, so models, rules engines, and audit trails are embedded in a way regulators and clinicians can understand.
Who benefits from tunable systems
- Clinical teams: Can tailor views, thresholds, and reports to their specialty and local protocols without waiting for a new release.
- Patients and carers: Get journeys, reminders, and recommendations that match their condition, abilities, and preferences instead of generic advice.
- Data and AI teams: Can safely adjust rules, cohorts, and model behaviour within controlled, auditable boundaries.
- Operations and management: Can experiment with configuration and pilots in specific sites before scaling across an organisation or region.
Design for renewable, sustainable health platforms
In healthcare, the only constant is change: clinical guidelines, reimbursement models, NHS standards, and privacy laws are all moving targets. Renewable healthtech software is designed so that you can safely update content, algorithms, and integrations without constantly rebuilding your core platform.
From a technical standpoint, this usually means modular architecture, clear boundaries between clinical content and code, and robust release processes for regulated environments. From a strategic perspective, it means accepting that your health app or platform is a long‑term product, not a one‑off project – and choosing a software development partner ready for ongoing iteration, not just initial delivery.
Renewability from different angles
- Clinical perspective: Clinical content, care pathways, and guidelines can be updated quickly as evidence changes, without waiting for a rebuild.
- Technical perspective: Modular architecture allows teams to swap or upgrade components (integrations, AI services, UI layers) with minimal disruption.
- Regulatory and governance perspective: Documentation, risk assessments, and audit trails are kept in sync with each release, supporting inspections and certifications.
- Organisational perspective: Change and transformation teams can plan continuous improvement cycles instead of one‑off, disruptive “big bang” go‑lives.
Better health data, better interventions
The value of custom healthcare software is increasingly measured in how well it turns raw data into actionable insight. Whether you are building remote monitoring tools, decision‑support systems, or hospital operations platforms, high‑quality data capture and interpretation are essential. In our article on how technology improves hospital operations, this shows up in task routing, transparency, and measurable time savings for clinical teams.
Regulators and clinicians care not only about what your AI or analytics engine predicts, but also how explainable and auditable those predictions are. This is especially important for software as a medical device (SaMD), where authorities expect clear evidence on intended use, performance, and post‑market surveillance. Building these capabilities into the product from the start makes it much easier to scale into new care pathways or markets later.
Different perspectives on data and AI
- Clinicians and multidisciplinary teams: Need data that is timely, accurate, and presented in a way that supports decisions rather than overwhelms them.
- Patients and carers: Want to understand what is tracked, how it is used, and how it benefits their care, with options to control or correct their information.
- Data, AI, and analytics teams: Require clear data governance, interoperability standards, and monitoring for bias and model drift over time.
- Commissioners and payers: Look for evidence that better data and analytics translate into fewer avoidable admissions, better outcomes, and sustainable costs.
Human‑centred design still wins
Even the most compliant app will fail if it ignores the people using it. Clinical staff operate in time‑pressured environments where poor UX quickly becomes a patient safety risk, not just an annoyance. Patients, on the other hand, often face accessibility barriers, health literacy challenges, and device or connectivity limitations that generic consumer UX patterns do not fully address.
Human‑centred digital product design for healthtech intentionally brings both groups into discovery and testing: co‑design workshops with clinicians, interviews with patients from different backgrounds, and regular usability checks in real clinics. Done well, this process helps you uncover what needs to be simple, what can be automated, and where human contact should never be removed from the care journey.
Who “human‑centred” really includes
- Patients, families, and carers: Interfaces, language, and support channels need to match different levels of health literacy, digital skills, and accessibility needs.
- Clinicians, nurses, allied health, and admin staff: Each group interacts with the system differently, so workflows and permissions must reflect their real tasks and constraints.
- Change and training teams: Need tools, content, and champions to help people adopt the product and fold it into everyday practice.
Inclusivity, safety, and trust by design
Because healthcare is a “your money, your life” category, both regulators and search engines look for signals of safety, transparency, and credibility. For your product, that means inclusive design, rigorous security, and clear consent flows; for your content, it means well‑structured articles, clear explanations, and transparent sourcing.
Inclusive healthtech software is tested with diverse populations – older adults, people with disabilities, users with low digital literacy – and updated when biases or gaps are identified. Trust also flows from how open you are about limitations: where AI is used, which guidelines you follow, and how patients can question or correct their data. These same themes appear in our overview of top types of healthcare software and trends, where responsible AI and equitable access are treated as core design principles.
Bringing it together for your next project
For health leaders planning new apps or platforms across the NHS and private sector, the most successful projects tend to share a pattern: they start with clinical doability, build tunable systems that can evolve, invest in renewable architectures, and treat data, UX, and inclusivity as one connected problem. Working with a custom software development company focused on MedTech and HealthTech helps keep all of these moving parts aligned from discovery workshops through to post‑launch optimisation.
Ready to build something that actually works for healthcare?
If you are planning a new digital health app or platform for the NHS or private sector and want to make it clinically doable, tunable, and sustainable, it helps to work with a team that has done it before.
At ULAM, the focus is on custom healthtech software development: from early discovery with clinicians and patients, through regulatory‑aware architecture, to long‑term iteration on real‑world outcomes. If you are ready to build something meaningful for healthcare, get in touch and let’s explore what we can create together.
Contact us to discuss your healthtech project




.svg)










.png)


















